Why You Should Be Paying Attention to the Emerging IgAN Market
A deep dive into a recent curiosity I had about the IgA Nephropathy (IgAN) market

Welcome back and thanks for continuing to read my work.
This week I decided to write about IgA nephropathy market. This one has been on my radar to investigate for some time for several reasons – and if its not yet on your radar, hopefully by the end of this piece you understand why this will be an important market for BioPharma moving forward.
Guess what, reader? Your sponsorship could go right here at the very top of the next Big Pharma Sharma post.
A sponsored post is 100% accessible to all subscriber levels and gets your brand, product, or service in front of my audience of BioPharma Industry decision-makers.
If you or your company is interested in becoming a Big Pharma Sharma sponsor, please reach out to me here or on my socials. Click the button below to learn how you can sponsor the next edition of Big Pharma Sharma.
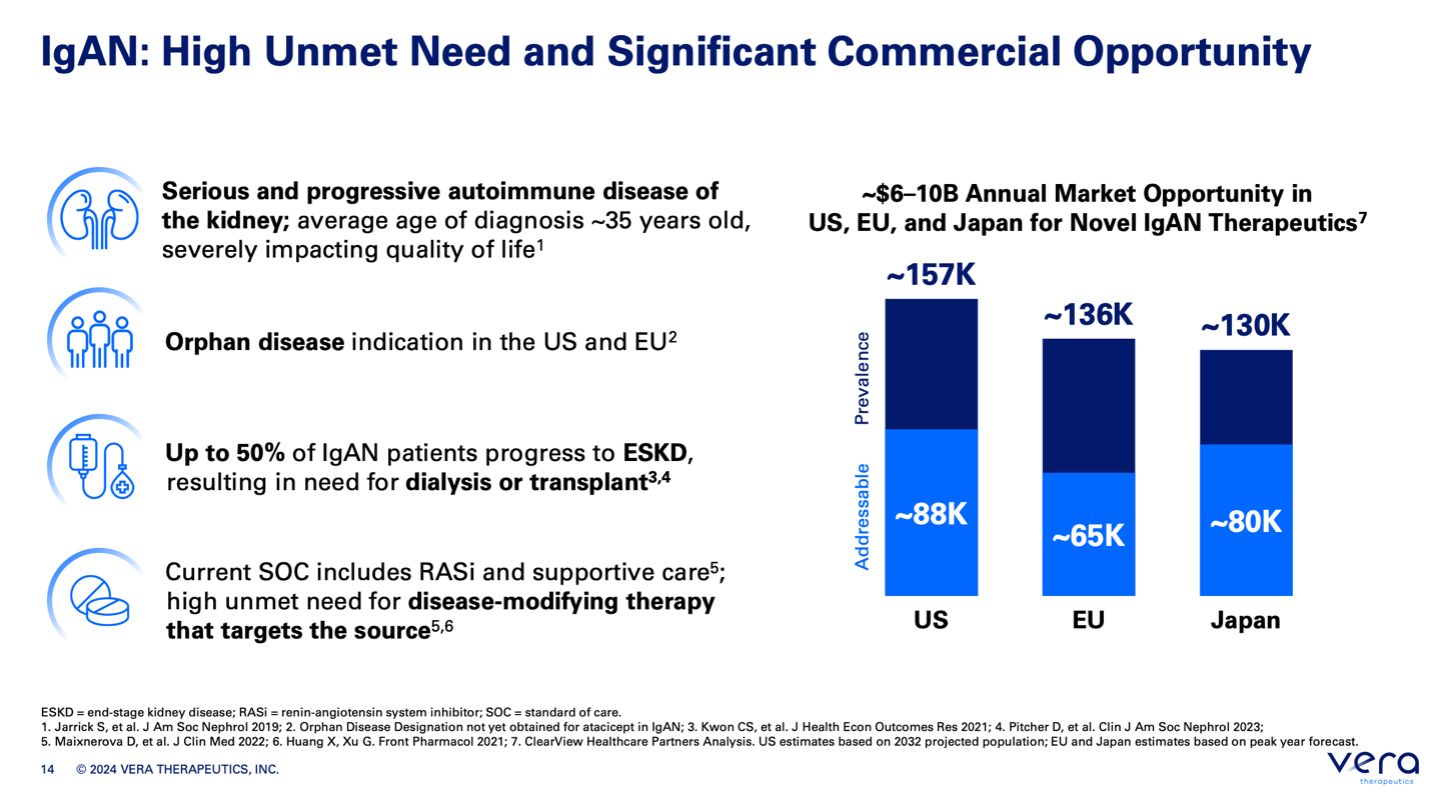
IgA nephropathy, also known as Berger's disease, is receiving great attention from the medical and pharmaceutical world because it is a potentially large and underserved market with high unmet need (see slide from Vera Therapeutics above). Patients are typically young (in their 20’s and 30’s) with ~50% progressing to end stage renal disease within 20 years and requiring dialysis. Once you’re on dialysis there’s almost no going back. Moreover, it is a huge expense to the healthcare system, so if you can treat patients early and modify disease such that you delay or minimize the need for dialysis treatment, you are offering a sizable lifetime benefit to patients and their health plans, and thus able to justify a relatively high price with payers. For example, TARPEYO (which we will get to later in the competitive landscape), is a targeted steroid (budesonide) with an annual cost of ~$194K.
The market is undeveloped as well, but projected to grow significantly as new treatments inch closer to approval, with some estimates guiding ~$15B in the US alone. Moreover, Big Pharma has already smelled green in this market, leading to a recent series of M&A, with Novartis, Biogen, and Vertex spending just shy of $10B over the last year to zero-in on IgAN as a key near-term revenue driver.
Current State of IgAN
Disease Overview
IgA nephropathy (IgAN), also known as Berger’s disease, is a common kidney disease that gradually damages the kidneys. It happens because the immune system mistakenly attacks the kidneys, leading to inflammation and scarring. This disease is caused by an abnormal form of a protein called IgA1, which is usually important for immune defense. In IgAN, the body makes antibodies against this abnormal IgA1, causing a chain reaction that damages the kidney filters (glomeruli). This damage leads to blood and protein leaking into the urine and reduces the kidney’s ability to clean the blood. Over time, many people with IgAN may develop kidney failure.
IgAN is the most common type of a group of kidney diseases called glomerulonephritis, which involve inflammation of the kidney’s filters. To diagnose IgAN, doctors need to do a kidney biopsy, which shows deposits of IgA in the kidney tissue.
People with IgAN can have very different symptoms. Some might not notice any symptoms and only find out through routine urine tests, while others may quickly develop severe kidney problems. The disease often goes undiagnosed or is recognized too late because not all regions use the same methods for testing.
Since there are limited treatments for IgAN, the main goal is to prevent kidney failure by managing symptoms, especially by reducing the amount of protein in the urine.
How IgAN Develops
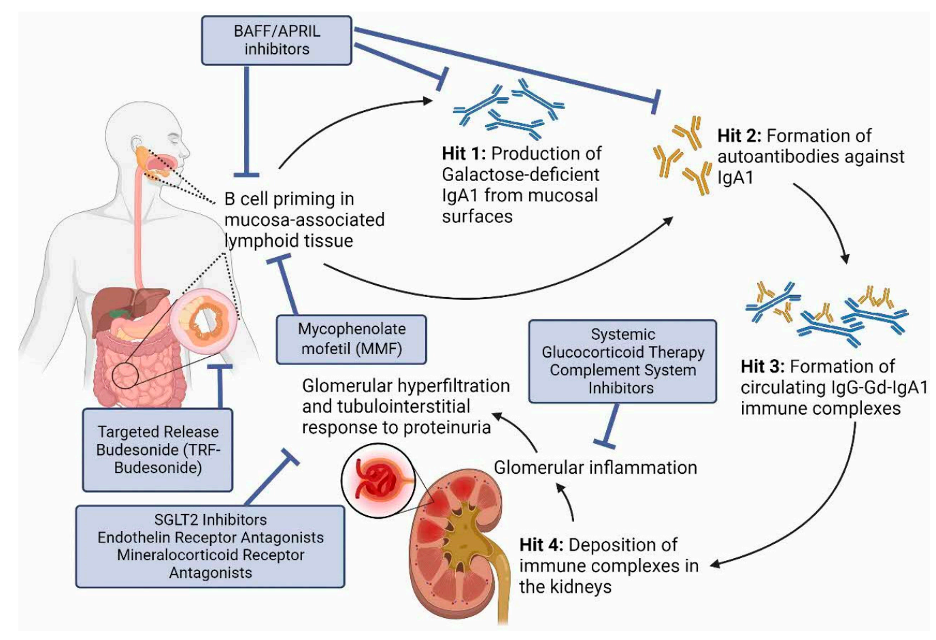
The “four hit hypothesis” is a nice framework for understanding the pathogenesis of IgAN and where in the disease path therapies under development are looking to target.
Hit 1: Abnormal IgA1
In people with IgAN, the IgA1 protein has an unusual structure. This abnormal IgA1 doesn’t have enough of a sugar called galactose, which makes it different from normal IgA1. About 70-80% of people with IgAN have high levels of this abnormal IgA1.
Hit 2: The Body’s Response
The immune system recognizes this abnormal IgA1 as something foreign and makes antibodies against it. These antibodies target the abnormal IgA1.
Hit 3: Immune Complexes Form
When these antibodies bind to the abnormal IgA1, they form large immune complexes. These complexes are too big to be cleared from the body easily and tend to get stuck in the kidney filters.
Hit 4: Inflammation and Damage
These large immune complexes get deposited in the kidney filters and cause inflammation. This inflammation makes the kidney cells release various chemicals that further damage the kidney tissue. This damage leads to protein and blood leaking into the urine, which are the main signs of IgAN.
Overall, these steps cause ongoing kidney damage, leading to the main symptoms of IgAN, which include blood in the urine and loss of kidney function over time. The repeated insults to the kidney lead to progressive damage that ultimately leads to needing dialysis.
Epidemiology
IgA nephropathy is technically a rare disease in the US but is the most prevalent form of primary glomerulonephritis globally, with a particularly high incidence in East Asia. It is estimated to affect 2.5 individuals per 100,000 population per year worldwide. The disease commonly presents in the second and third decades of life and exhibits a higher incidence in males, with a male-to-female ratio of approximately 2:1. Family clustering of the disease suggests a genetic component, supported by various genome-wide association studies.
Current Treatment Landscape
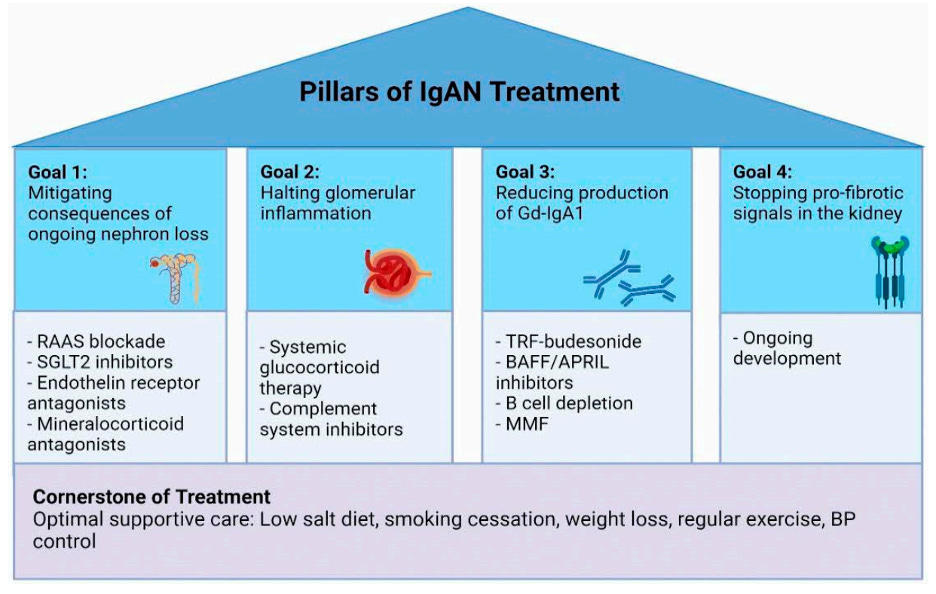
The primary goals of treatment in IgA nephropathy are to manage symptoms, reduce proteinuria, control blood pressure, and slow the progression of kidney damage. If you’d like to get more into the weeds about the treatment flow of a typical IgAN patient, I learned a lot from AJKDblog.org.
Below I’m just going to go through some of the key interventions at a very high level. The following are key components of the current treatment guidelines. As you’ll see, the main goal of intervention here is to preserve kidney function, as evidenced by a reduction in proteinuria and stabilization of estimated glomerular filtration rate (eGFR). This is all ideally happening on backbone of optimal lifestyle changes, like reducing sodium intake, smoking cessation, weight loss, and exercise.
Blood Pressure Control:
ACE Inhibitors (ACEIs): Drugs like enalapril and lisinopril are commonly prescribed to lower blood pressure and reduce proteinuria.
Angiotensin II Receptor Blockers (ARBs): Medications such as losartan and irbesartan are used similarly to ACEIs to control blood pressure and decrease proteinuria.
Renin-Angiotensin System (RAS) Blockade:Combined use of ACEIs and ARBs is sometimes considered, although the risk of hyperkalemia and renal dysfunction necessitates careful monitoring.
SGLT-2 inhibitors: Drugs like dapagliflozin and empagliflozin, initially used for diabetes have shown the ability to reduce proteinuria and preserve eGFR in subgroups of CKD patients with IgAN
Endothelin Blockade: One of two approved drugs for IgAN, specifically. This is a targeted-release reformulated steroid that has shown benefit on proteinuria and eGFR. Sparsentan is an endothelin type A receptor (ETA-R) and angiotensin receptor antagonist. In February 2023, the FDA granted accelerated approval to sparsentan as the first non-immunosuppressive medication for treating adults with primary IgAN.
Immunosuppressive Therapy:
Systemic Corticosteroids: Prednisone is often used in patients with persistent proteinuria (>1 g/day) despite optimized RAS blockade. The typical regimen involves high-dose prednisone for 6-8 weeks, followed by a taper. Physicians seem to avoid using this if possible due to AEs
Budesonide: One of two approved drugs for IgAN, specifically. This is a targeted-release reformulated steroid that has shown benefit on proteinuria and eGFR. It contains a pH-sensitive capsule that targets delivery of the steroid to the ileum.
Despite these treatment strategies, many patients with IgA nephropathy continue to experience disease progression, highlighting the need for new and more effective therapeutic options.